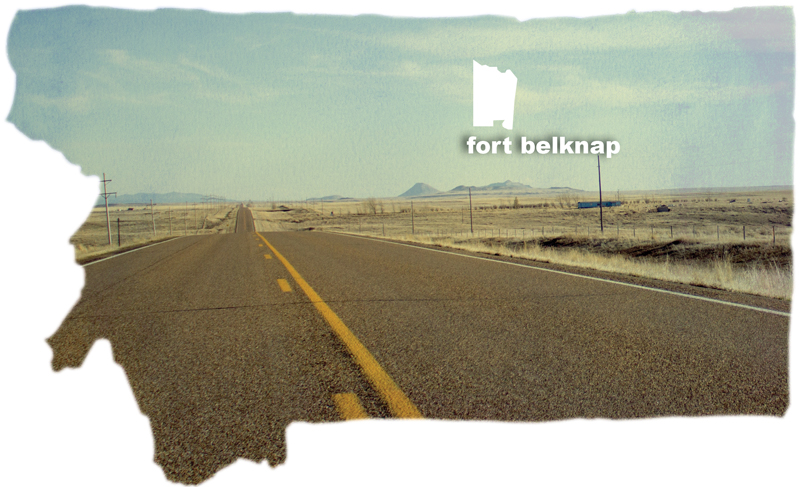
Fort Belknap
Fort Belknap – Flipping the Coin
- The sun sets over the Fort Belknap reservation, the shared home of the Assiniboine and Gros Ventre tribes.
- Jack Plumage sits in his living room while his granddaughter’s friends retrieve some snacks from the kitchen. Plumage is one of relatively few American Indians in Montana who has the benefit of Medicare and Veterans Affairs to cover what the Indian Health Service cannot.
- Plumage reaches into his refrigerator to retrieve his insulin. He takes around a dozen pills a day to manage his health and to keep his transplanted kidney functioning.
- Patty Getten works in the Tribal Insurance Department and says she will not sign up for Medicaid or any form of health care outside of the Indian Health Service. She wants the health care and education pledged by the federal government in the original treaties. Getten plans to rely on what was promised, even though she blames the Indian Health Service for mistreating her mother’s diabetes, which Getten believes led to her death.
- Plumage, 66, has run a long health gauntlet. He has had diabetes since 1984 and suffered from a stroke in 1996. A tumor wrecked one of his kidneys while his diabetes ravaged the other, leaving him to rely on dialysis until his sister, Jill Plumage, donated one of her kidneys.
- Patty Quisno, 72, is the River Gros Ventre representative on the Fort Belknap Community Council and a former Indian Health Service employee. Quisno now provides oversight for tribal health entities on the reservation, other than the IHS. She is covered by Medicare and the private insurance she kept after retiring from IHS.
- Manuel Morales is the USDA program director at the Aaniiih Nakoda College. A $100,000 annual grant from the United States Department of Agriculture funds a two-and-a-half-acre community garden and greenhouse. The garden is a preventative health care effort in collaboration with the Fort Belknap Diabetes Prevention Center, Healthy Hearts, the tribal health center and the Indian Health Service.
- Fort Belknap Agency as viewed from one of the town’s two water towers. This reservation is one of the poorest places in Montana. Seventy to 80 percent of residents are unemployed and rely on government assistance or temporary jobs passing through. To the right is the Milk River, and the large, red-roofed building in the center is the reservation’s main Indian Health Service facility.
- Ethel Bear works at Fort Belknap Agency’s tribal health center, an Indian Health Service funded offshoot facility. Bear is responsible for patients’ third-party billing, which brings money back into the IHS by billing a patient’s insurance, such as Medicaid, if they have it.
- An anonymous grave site at a cemetery off Highway 2 on the Fort Belknap reservation makes death seem a little closer here than elsewhere. The average life expectancy for American Indians living on Montana reservations is 67 — markedly lower than the United States average of 77.

Jack Plumage sits in his living room while his granddaughter’s friends retrieve some snacks from the kitchen. Plumage is one of relatively few American Indians in Montana who has the benefit of Medicare and Veterans Affairs to cover what the Indian Health Service cannot.
Story by TAYLOR W. ANDERSON
Photographs by HUNTER D’ANTUONO
Jack Plumage died once, but he’s one of the lucky ones.
He’d had a stroke and lay in his hospital bed when he died. He remembers having a vision before coming back, he says, five hours later.
He’s 66 now. That’s not considered particularly old. Not in most places in the country. But for a Native American living on one of Montana’s seven reservations, he’s close to the horizon of the average life expectancy of about 68.
Plumage has one kidney. His left one died from diabetes and was replaced by his sister’s kidney. The right one got a tumor on it, so it had to go.
“I went through surgery on a Friday, and they were just gonna take out three millimeters, it wasn’t that big,” Plumage says. “Then they decided they’d just take the whole kidney out. It might have spread, so they took it all out.”
Plumage is lucky because he can access the country’s health care system without having to go through the Indian Health Service. The system is in place to provide health care, as mandated in federal treaties with the nation’s 565 recognized tribes. But in Montana, it is underfunded and understaffed, unable to provide for people like Plumage and others.
Plumage, a descendant of both tribes on the Fort Belknap reservation, the Gros Ventre and Assiniboine, is a veteran, and for three decades his aging, muscular body has been in and out of health clinics across the Northwest for dialysis, transplants and diagnoses not provided on the Fort Belknap Indian Reservation in northcentral Montana.
About 40 percent of Montana’s Native Americans are uninsured, according to Montana Budget and Policy Center estimates, meaning a significant number of tribal members rely solely on the IHS.
Services such as child delivery and operations need to be outsourced to off-reservation clinics in nearby Havre, 47 miles away, and as far away as Billings, about 200 miles away from Fort Belknap Agency.
Put simply, the IHS needs more people like Plumage, the man with one kidney who doesn’t believe he could have survived this long on local IHS care alone. Having Medicaid and later Medicare and Veterans Affairs insurance allowed Plumage to get the care not provided near this 40-miles-by-30-miles prairie landscape reservation. It also didn’t cost the IHS a dime.
It’s common for the Fort Belknap Health Center to send patients to doctors in off-reservation towns for the care that can’t be provided in the clean brick-and-mortar facility in the middle of the crumbling Agency roads. When a Native American patient without insurance uses the IHS, the federally funded program is responsible for the bill.

Plumage, 66, has run a long health gauntlet. He has had diabetes since 1984 and suffered from a stroke in 1996. A tumor wrecked one of his kidneys while his diabetes ravaged the other, leaving him to rely on dialysis until his sister, Jill Plumage, donated one of her kidneys.
Nationwide, the IHS can’t afford the need, so without insurance, Native Americans face grim health care scenarios.
In terms of people as dollars, patients in need of immediate treatment are costly, and there isn’t enough money for preventative care. Plumage won’t use the IHS anymore. He doesn’t have to. He gets his pills there, but that’s about it. He is insured and can drive west along the Montana Hi-Line and lazy Milk River to Northern Montana Hospital in Havre, 45 minutes away.
In the living room of his home in Fort Belknap Agency, with family pictures on the walls and family members sleeping upstairs and others playing downstairs, Plumage lifts his shirt to expose a deep and reddened scar. It runs down his stomach. Given his daily diet of insulin and pharmaceuticals, today, Plumage is lucky to be alive.
“There’s been a lot of changes that I see in the IHS, from recruiting to care to all that,” he says. “And a lot of the Indian people here, they don’t realize that they should be getting better care. They really should. That’s all they got when they go there.”
People on Montana’s seven reservations die younger than many others around the country. They’re getting diabetes at an alarming rate. They have less money to live on, and the dollar has to go further at the grocery store or gas station. That means the processed foods at the Albertsons in Harlem make up a good portion of diets on this reservation.
Many on and near Fort Belknap are overweight and at risk of diabetes and other diseases. Parents are increasingly concerned with the obesity rates in schools. “Nearly 60 percent of the students are in the abnormal weight category,” said Julie King Kulbeck, who runs the tribally managed Diabetes Prevention Program.

Jack Plumage reaches into his refrigerator to retrieve his insulin. A diabetes patient since 1984, he takes around a dozen pills a day to manage his health and keep his transplanted kidney functioning.
Plumage is one of the 60 percent of Native Americans in Montana who have health insurance. Most people between the ages of 18 and 64 are uninsured, another national high among Native people. About one-in-five have private insurance, according to the Montana Budget and Policy Center.
In Montana, Native Americans rely heavily on the IHS for care, checkups, physicals and pharmaceuticals. Leslie Racine, a planning officer at the regional Billings IHS office, said the region has funding for about a quarter of the need.
According to a report filed this year, funding for the Billings IHS office decreased by a little more than a million dollars from 2012-2013. In it’s 2014 budget justification, the office is seeking to recoup that shortfall in its requested $66.5 million.
American Indians and Alaska Natives are six and a half times more likely to die from alcohol-related illness than any other U.S. races; almost three times as likely to die from diabetes and twice as likely to be murdered or die unintentionally, according to IHS mortality disparity rates.
Waiting times in the state’s IHS clinics are high. There aren’t enough doctors or nurses to provide prompt care. The doctors who come don’t stay long. They don’t want to live anywhere near this rural reservation, says tribal councilwoman Patty Quisno. They’ll come fresh from school and stay for a few years before moving on. They come because working for IHS forgives $20,000 per year in student loans for up to two years of service at the clinics.
In mid-April, there were 103 openings at IHS clinics throughout Montana. Another 10 were open in Wyoming. Jobs pay well, much more than the average wages made by the 20-30 percent who are employed on Fort Belknap.
A doctor came a few years ago from New York and another from West Virginia. Plumage liked the doctor from West Virginia, and the doctor liked it here. His wife didn’t. So they moved back east, and the IHS facility here had an open position again. Today, it has open positions for medical officers, nurses, lab technicians and pharmacists.
Plumage says the facilities around here aren’t hospitals. Hospitals birth babies and treat cancer patients and perform surgeries and typically have more patients than administrators. These facilities are clinics; Armories, as Plumage calls them.

An anonymous grave site at a cemetery off Highway 2 on the Fort Belknap reservation makes death seem a little closer here than elsewhere. The average life expectancy for American Indians living on Montana reservations is 67 — markedly lower than the United States average of 77.
“Indian Health used to be, not saying it isn’t today, but it used to be a lot better in my opinion,” Plumage said. “A lot better staffed, they had an ambulance crew.”
He would know. He used to be the Fort Belknap service unit director. He was also tribal chairman once.
Plumage worked for the Bureau of Indian Affairs on Fort Belknap in the 1980s when his physical tests spotted diabetes, the disease that would lead to a failing pair of kidneys, sending him away to the big hospitals in Oregon.
More recently, it was the cancer that sent him back to Portland. The doctors found a tumor on his right kidney in 2012 and decided to take the whole thing out. After battling an abscess after the surgery, Plumage has been feeling better.
Because he was insured, Plumage saved a big chunk of money for the Indian Health Service’s Contract Health Service, which coordinates health care coverage for tribal members treated in off-reservation facilities.
He’d probably have ranked high on the Contract Health Service referral list—a 12-tiered ranking system for judging who can’t wait to get to a hospital. “I usually just go to the VA whatever troubles me,” Plumage said.
The VA bought Plumage plane tickets just fine, but it wouldn’t reimburse him for the train tickets he bought for trips to doctors throughout the Northwest. He liked going through Glacier National Park on the train anyway, and the track follows the Hi-Line and Route 2 through the plains of eastern Montana.
He ended up paying for some train tickets and a knee surgery. A combination of Medicare, VA and the IHS has paid for everything else he’s needed.
For those without insurance here, they have to either work or pray for health, or hope to make it onto the list for referral out of the IHS and into the Northern Hospital in Havre to see a doctor in a facility with more services.
Leslie Racine, the Billings IHS planning officer, put it another way. “We have to have one foot in the grave before they send us out,” she said.
The IHS can’t afford to send everyone to see a doctor off the reservation, so an IHS committee uses the 12-step evaluation to see who the Contract Health Service should send to the doctor on its tab and who can wait. Appeal times are slow, and it’s the waiting they’re sick of, and maybe sick from.
Administrators wait and see how much the federal government will give them, and then they adjust funds. If there are cuts, as there may be next year, fewer patients will get to the doctors off reservations, and more will wait.
Many here are poor. Seventy to 80 percent don’t have work and wait on either temporary jobs passing through with the seasons or government assistance.
There’s a casino, gas station and no hotel on Fort Belknap. The largest employer is the tribal government. But even council delegates aren’t much different than unemployed residents.
Councilors sat in chambers on a Tuesday, waiting for a quorum to arrive to start the meeting. Tribal President Tracy King was there, patched up after a run-in on the road with a cow. He didn’t have insurance either at the time of his accident, and he said health care is an issue that should be addressed here.
The council knows the residents are suffering, and some express valid interest in addressing the issue from a leadership position.

Patty Quisno, 72, is the River Gros Ventre representative on the Fort Belknap Community Council and a former Indian Health Service employee. Quisno now provides oversight for tribal health entities on the reservation, other than the IHS. She is covered by Medicare and the private insurance she kept after retiring from IHS.
“What we talked about was taking their Contract Health dollars, which is probably several million dollars, just taking that money and converting it to a universal reservation insurance policy, which would cover everybody,” Quisno said.
President King, Buster Moore, Andy Werk and other tribal councilmembers agreed: There needs to be a better way for tribal members to seek care. But that’s a long way off.
Quisno worked for the Indian Health Service for 34 years before retiring in 1994. She’s kept her private insurance after leaving the IHS, and she has Medicare. Some older residents here have that. The elderly typically use the health system more and cost more money to care for, and the IHS encourages people to sign up for Medicare.
Patients with insurance help earn IHS revenue, as the program bills treatment costs to insurance companies and health programs like Medicaid. The IHS expects to collect about $120 million more next year from billing Medicaid, Medicare and private insurers, mostly because the 2010 Affordable Care Act expanded Medicaid in a number of states.
Kevin Howlett, head of the Flathead reservation’s tribal health department, said more insured Native Americans is only one side of the coin. “There’s a whole host of factors, and one thing I emphasize across the state is it doesn’t do any good to get people on Medicaid if they go right by your clinic.”
Howlett’s program is one of two on reservations in Montana where the tribe runs its own department aside from the IHS, which Howlett says improves care for people.
“IHS as an institution is more concerned with the preservation of the institution, rather than the status or improving the health of Indians,” he said.
About 43 percent of Native Americans in Montana either have Medicare, Medicaid or private insurance. If more patients both had insurance and used the clinics on reservations, it would generate revenue and keep money from flowing out of the IHS’s limited budget, leading to more money for improved care for Native Americans throughout the state.
Something has to change. For patients who use the IHS, there’s nowhere else to go.

Ethel Bear works at Fort Belknap Agency’s tribal health center, an Indian Health Service funded offshoot facility. Bear is responsible for patients’ third-party billing, which brings money back into the IHS by billing a patient’s insurance, such as Medicaid, if they have it.
The young people from Fort Belknap typically aren’t born in Fort Belknap anymore.
Plumage says his daughter was one of the last born in the Fort Belknap hospital before it was torn down and replaced by the current clinic, just a few blocks from his house.
The Fort Belknap service unit lost accreditation to deliver babies years ago. It couldn’t afford it. Keeping a doctor on staff for the few deliveries each month wasn’t worth it. Now, pregnant Native Americans are asked to apply for Medicaid before they are referred elsewhere. If they are denied Medicaid, the IHS will pay for the pregnancy care.
Relatively few Native Americans in this state have Medicaid, the state- and federally funded program for low-income people. It’s clear many are qualified. The average Native American in Montana made about $26,000 a year, about $16,000 less than whites.
Many Native Americans are eligible but either don’t know or don’t want to enroll in the federal program. In her office in the diabetes center, Kulbeck said she didn’t have insurance because she couldn’t afford it, and she didn’t think she was eligible because she was working. But she didn’t know whether she would meet the eligibility requirements. Under Montana’s stingy Medicaid eligibility limitations, she probably wouldn’t, but she doesn’t know.
Twenty thousand more Native Americans would have been eligible if the state decided to expand Medicaid under the Affordable Care Act. With so many residents on Fort Belknap out of work, it’s safe to say many would have met the expanded 138 percent poverty threshold. But, in April, a conservative state Legislature decided it would wait and spend two years reforming what it considers a broken system.
There are three parties around Fort Belknap when it comes to stances on Medicaid: the one that has it or is eligible for it, the one that isn’t eligible to be on it, and the one that doesn’t want to be on it.

Patty Getten works in the Tribal Insurance Department and says she will not sign up for Medicaid or any form of health care outside of the Indian Health Service. She wants the health care and education pledged by the federal government in the original treaties. Getten plans to rely on what was promised, even though she blames the Indian Health Service for mistreating her mother’s diabetes, which Getten believes led to her death.
Patty Getten works in the Tribal Insurance Department, and she’ll never be on Medicaid. Her mother had diabetes and was on Medicaid. Her husband has had two heart attacks. But she says she won’t pay for what’s owed to her, referring to the federal treaty rights to health care promised to the nation’s tribes. “As long as the water flows and the grass is green, I’ll get my health care from the IHS,” she says.
What’s important to people here doesn’t seem to be that they’re dying.
The IHS keeps people alive, but it’s going to get tougher when federal budget cuts sink in deep. The clinics were already cut back. Unless something changes and more people get lucky like Plumage, the system will fund fewer patients annually.
The people will continue waiting for preventative care. They’ll keep dying, and unless the people can have ready access to the hospitals in Havre and elsewhere, they may die faster.
Plumage isn’t dead yet. He struggles off his couch to his feet and walks around his house. Plumage lives.
 Native News Project 2013
Native News Project 2013